The state of Florida is trying out a new approach to measles control: No one will be forced to not get sick.
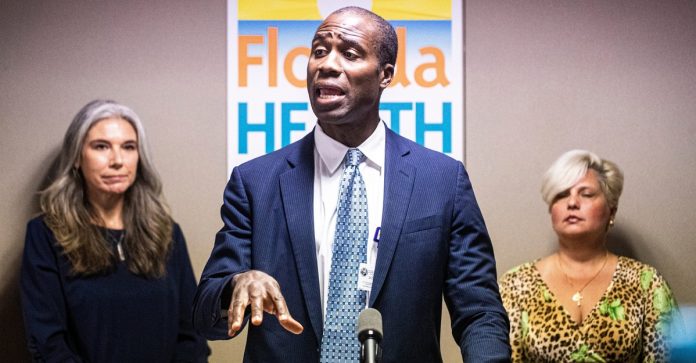
Joseph Ladapo, the state’s top health official, announced this week that the six cases of the disease reported among students at an elementary school in Weston, near Fort Lauderdale, do not merit emergency action to prevent unvaccinated students from attending class. Temporary exclusions of that kind while an outbreak is ongoing are part of the normal public-health response to measles clusters, as a means of both protecting susceptible children and preventing further viral spread. But Ladapo is going his own way. “Due to the high immunity rate in the community, as well as the burden on families and educational cost of healthy children missing school,” he said in a letter released on Tuesday, the state’s health department “is deferring to parents or guardians to make decisions about school attendance.”
That decision came off as brazen, even for an administration that has made systematic efforts to lower vaccination rates among its constituents over the past two years. Ladapo’s letter acknowledges the benefits of vaccination, as well as the fact that vulnerable children are “normally recommended” to stay home. Still, it doesn’t bother giving local parents the bare-minimum advice that all kids who are able should get their MMR (measles, mumps, and rubella) shots, Dorit Reiss, a professor and vaccine-policy expert at UC Law San Francisco, told me: “I wouldn’t have expected him, in the middle of a measles outbreak, to be willing to sacrifice children in this way.”
The Florida Department of Health has not responded to a request for comment on Ladapo’s future plans, should this situation worsen. For the moment, though, he has chosen to lower the guardrails from their standard height. It’s an escalation of his, and Florida’s, broader push against established norms in public health, especially as they relate to vaccination. So what happens now?
At least in any immediate sense, Ladapo’s decision may not do much harm. In fact, there’s good reason to believe that its effects will end up being minimal. Parents who have children at the school, Manatee Bay Elementary, have until today to decide whether to pull out those kids for the next three weeks. Many seem to have already done so: About 200 students and six teachers have been absent, according to local news reports. In the meantime, Broward County Public Schools’ superintendent said yesterday that just 33 students out of the school’s nearly 1,100 were still unvaccinated. Given those two facts—some degree of self-imposed isolation, and 97 percent of the community now having some level of immune protection—the virus will have a hard time spreading no matter what the rules for attendance might be.
Disease modeling, too, suggests that the risk of a larger outbreak is low. For a study released in 2019, a team of researchers based at Newcastle University and the University of Pittsburgh simulated thousands of measles outbreaks at schools in Texas, the most populous state to allow nonmedical exemptions from routine vaccine requirements. The researchers looked at the extent to which a policy of sequestering unvaccinated kids would help to reduce the outbreaks’ size. In the median outcome, even without any school-wide interventions, they found that an initial case of measles spreads only to a small handful of people. Adding in the rule that unvaccinated kids must stay at home has no effect on transmission. When the school’s vaccination rates are assumed to be unusually low, the rule reduces the outbreak’s size by one case.
Not all of the modeling outcomes are so rosy. For the very worst-case scenarios, in which a case of measles emerges in a school where unvaccinated kids happen to be clustered, the study found that forced suspensions have dramatic benefits. A major outbreak in the Dallas–Fort Worth area, for example, might end up infecting 477 people in the absence of any interventions, according to the model. When unvaccinated kids are kept from going to school, that number drops by 95 percent.
Hypothetical models can’t tell us what will happen in a real-life school with real-life kids, like the one in Weston, Florida. But given Manatee Bay Elementary’s reported vaccination rate, it’s fair to assume that Ladapo’s policy won’t be catastrophic. Indeed, it may well end up sparing a few dozen families from the fairly serious inconvenience of being out of school without having much effect at all on the outbreak’s final size.
But is the sparing of that inconvenience worth the risks that still remain? (And how should one value the time of a parent who could have vaccinated their child but chose not to?) As Reiss points out, if this policy leads to even one more case in the current outbreak, it will have put one more kid at risk of hospitalization, long-term complications, or even death. Worst-case outbreak scenarios do occur from time to time, as we all know well by now, and the Weston outbreak getting much worse is certainly within the realm of possibility. Any public-health authority would have to weigh these odds in the face of a six-case cluster, and surely almost every statewide health authority would choose to err on the side of caution. In Florida, though, the scale appears to tip the other way: Ladapo has rolled the dice on doing less.
That’s been his way since the very day he was appointed by Governor Ron DeSantis, in September 2021. Just hours after he was introduced, the state ended mandatory quarantines for low-risk students who had been exposed to COVID. The following March, just a few weeks after being confirmed into the job, Ladapo announced that Florida would be “the first state to officially recommend against the COVID-19 vaccines for healthy children.” He continued to scale up from there: That fall, he recommended against the use of mRNA vaccines by any men under the age of 40. A year later, in October 2023, his office warned everyone under the age of 65 about the risks of getting an mRNA-based COVID booster. And then, finally, just last month, Ladapo came out with a warning that mRNA-based COVID vaccines “are not appropriate for use in human beings.”
The man’s commitment to undermining vaccination is truly unparalleled among leading public-health officials. “As a surgeon general he stands alone,” Reiss told me. Yet Ladapo’s policy activism, however grotesque it might seem, has been bizarrely ineffective in practice. Take his March 2022 move to lead the way on not vaccinating young people against COVID. Media coverage of that announcement dwelled on reasonable concerns that this policy would dampen immunization rates; vaccine experts said it was a dangerous and irresponsible move that would “cause more people to die.” In practice, though, it seems to have done almost nothing. At the time of Ladapo’s announcement, 24.2 percent of Florida’s kids and 66.3 percent of its teenagers had received at least one dose of a COVID vaccine. (The corresponding national numbers at the time were somewhat higher.) By the end of the year, and in spite of Ladapo’s contrarian guidance, Florida’s vaccination numbers for these age groups were up by about four and three points, respectively—which is almost exactly the same amount, percentage-wise, as the increases in those numbers seen across the country.
Or compare Florida’s experience to that of Nevada, a state that had very similar child and teen vaccination rates in March 2022: 23.1 percent and 64.0 percent. Through the end of 2022, while Ladapo was discouraging his constituents from getting shots, that state’s Democratic governor was engaged in a large-scale effort to do the opposite. Yet the results were essentially the same: Nevada’s rates increased by pretty much the same amount as Florida’s.
For all of Ladapo’s efforts to dampen his state’s enthusiasm for life-saving interventions, Florida’s age-adjusted rates of death from COVID do not appear to have increased relative to the rest of the country, at least according to reported numbers. In this way, one of the nation’s loudest and most powerful voices of vaccine skepticism seems to be shouting into the wind. His proclamations and decisions to this point have been exquisitely effective at producing outrage but embarrassingly feeble when it comes to changing outcomes. Even taken on its own terms, as a means of changing public-health behavior, Ladapo’s anti-vaccine activism has been a demonstrable failure.
Perhaps this week’s decision to relax the rules on fighting measles will mark just one more step along that path: Once again, Florida’s surgeon general will have taken an appalling stance that ends up having no effect. But then again, now could be different. By the time Ladapo got around to undermining COVID shots, more than two-thirds of the state’s population, and 91 percent of its seniors, were already fully vaccinated. The damage he could have done was limited. But the measles outbreak in Weston is unfolding in real time. More such outbreaks are nearly guaranteed to occur in the U.S. in the months ahead. Reiss worries that Ladapo’s new idea, of choosing not to separate out unvaccinated kids during a school outbreak, could end up spreading to other jurisdictions. “If this becomes a precedent, that becomes a bigger problem,” she told me.
For the first time since taking office, Ladapo may finally have a real opportunity to make a difference through his vaccination policy. That’s a problem.
Source link
Daniel Engber